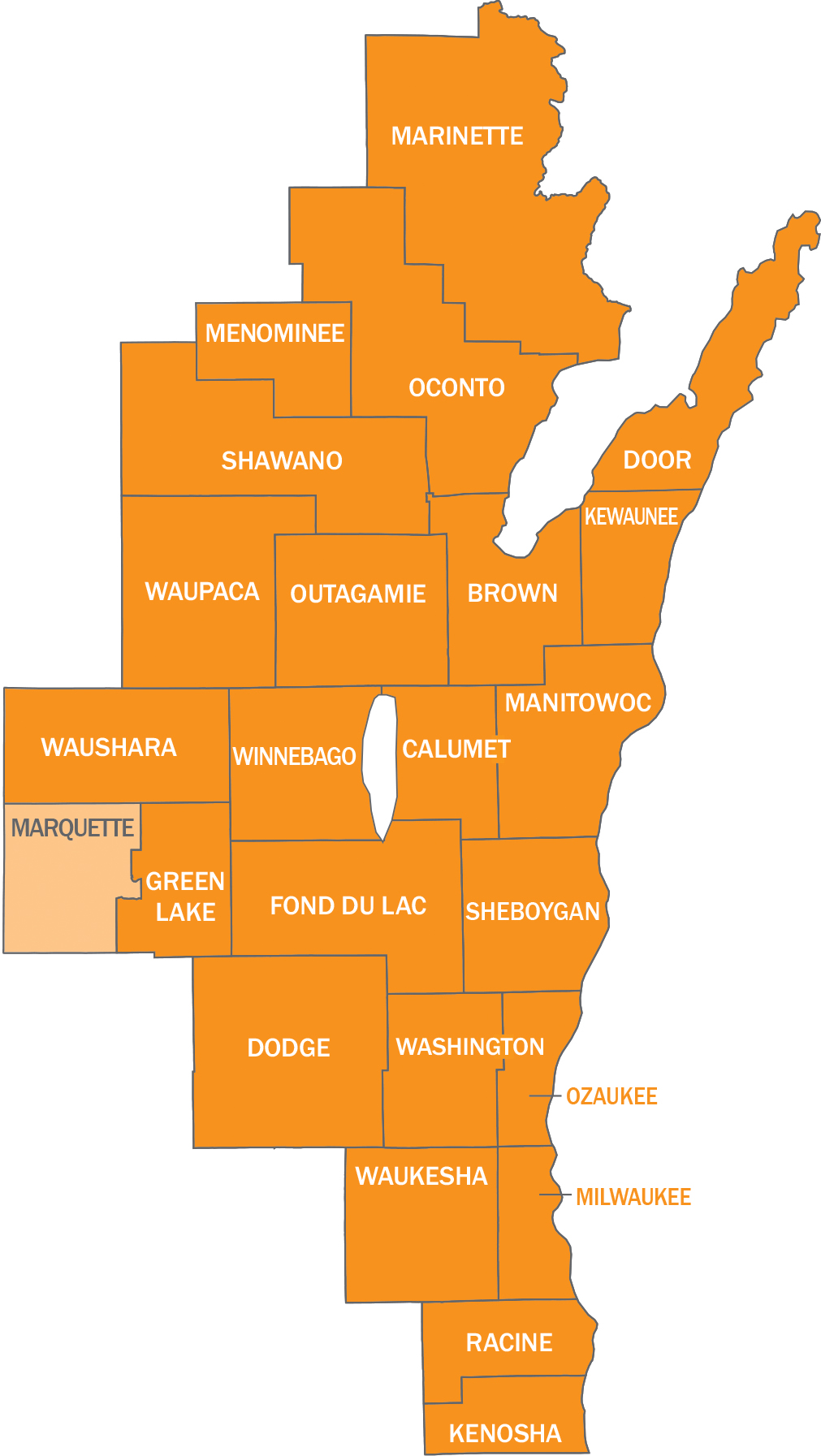
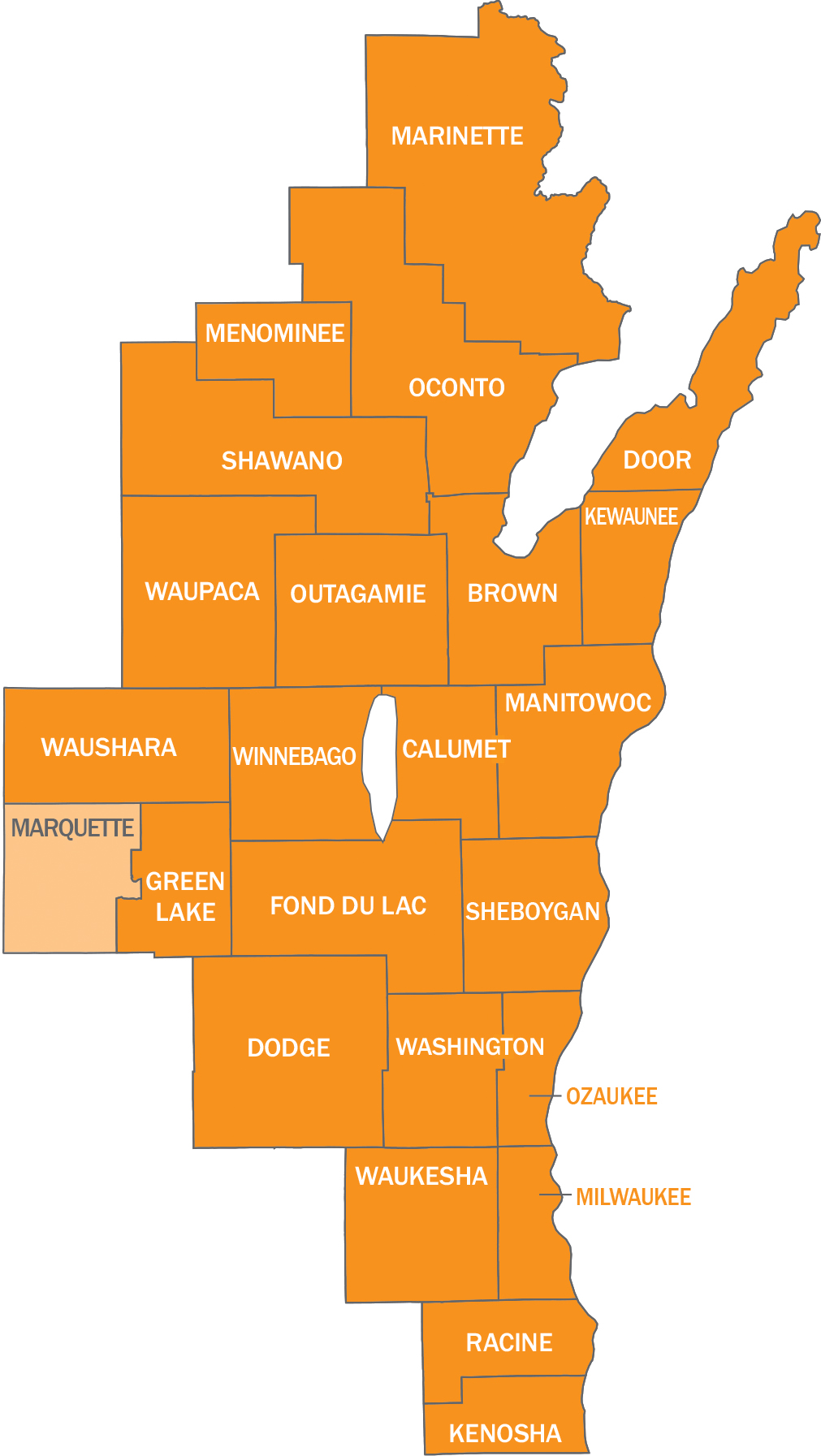
Service Area
To enroll with Network Health, click on the Enroll Now button below. Follow the enrollment instructions and select Network Health as your health plan. You can also download the Health Insurance Application/Change Form and complete it. Under Choose a Health Plan, write Network Health. Return the completed form to your employer.
When it comes to offering access to local, high-quality providers and health systems, Network Health is a smart choice. We have Froedtert & the Medical College of Wisconsin, ThedaCare Health, Ascension Wisconsin, Children’s Wisconsin, ProHealth Care hospital and clinic locations as of August 1, 2025 and Aurora Health Care beginning January 1, 2026, all in-network. This strong network helps ensure the best care possible is available to you. To learn more about Network Health and what we can offer, scroll down or click on the links below.
At Network Health, we do what’s right, even when it isn’t easy. We’re honest and hardworking, just like you. That’s why we take the extra steps to make health insurance affordable and understandable.
For over 40 years, Network Health has been going above and beyond for State of Wisconsin employees, putting members first and helping improve their lives and those of their families. As the top-rated plan for quality, Network Health provides access to care for your whole family, right around the corner.
See what makes us a different kind of health insurance company – download this brochure. If you still have questions or are looking for more information, scroll down or give us a call at 844-625-2208.
The State of Wisconsin Group Health Insurance Program has a dedicated phone line to handle your questions or concerns. Your calls go to our local member experience team, who will be able to address any questions or concerns you may have.
To speak with a specially trained Network Health representative, call 844-625-2208 or 920-720-1811. Our member experience team is available Monday - Friday from 8 a.m. to 4:30 p.m. You can also email us a question by using our Contact Us form.
Have questions regarding Network Health's State of Wisconsin Group Health Insurance Program? Check out our list of frequently asked questions and get your questions answered right now.
Network Heath’s provider network is combined across northeast and southeast Wisconsin. We have Froedtert & the Medical College of Wisconsin, ThedaCare Health, Ascension Wisconsin, Children’s Wisconsin, ProHealth Care hospital and clinic locations as of August 1, 2025 and Aurora Health Care beginning January 1, 2026, all in-network. This strong network helps ensure the best care possible is available to you. Our network includes the following high-quality major health systems (among others).
Froedtert & the Medical College of Wisconsin
ThedaCare Health
Children’s Hospital of Wisconsin (including Appleton, Green Bay, Milwaukee and Neenah)
Ascension Wisconsin
Aurora Health Care New starting January 2026.
Bellin Health
Prevea Health
SSM Health
ProHealth Care New starting August 2025.
To confirm your doctor is an in-network provider, go to networkhealth.com/find-a-doctor and click on the Start Your Search button. Sign in by choosing a plan or use your existing plan to sign in. Then choose State of Wisconsin employees/members when asked to select a plan type.
Go to our Find a Doctor search tool.
Enter your location and then select State of Wisconsin employees/members as your plan.
Choose how you want to search - by doctor name, doctor specialty or facility name - and enter your search criteria.
You can also download a PDF of the provider directory. If you would like a printed directory mailed to you, please call 844-625-2208.
*Please note – Both the provider AND the provider facility must be in-network and located in Network Health’s service area for medical services to be covered by your Network Health benefits plan.
Network Health offers a variety of unique and helpful benefit extras with all our State of Wisconsin Group Health Insurance plans.
Health Management Services
Care Management - Personalized coordination of care, access to care, identification of benefits and resources, and condition monitoring
Condition Management - One-on-one health coaching about ongoing care for specific chronic conditions
Breathe At Ease Program - Proactive program to help participants avoid flare-ups, control symptoms and potentially improve their lung conditions
Prevent T2 Lifestyle Change Program - Program for people with prediabetes and who are at high risk for type 2 diabetes and want to lower their risk
Learn More About Benefit Extras
Check out the links below for more information on your dental, pharmacy and wellness benefits.
Network Health's mission is to create healthy and strong Wisconsin communities. We live and work in the same communities as our members and we care about making our homes a better place to live. We do this by investing in our community through volunteering, hosting events, sponsoring events and donating to local organizations.
Visit our Community Engagement web page where you will find a variety of resources and information.
How to get involved
Upcoming events
How to partner with Network Health for volunteer opportunities
Community partner spotlight
Network Health's annual report
Network Health complies with applicable Federal civil rights laws, conscience and anti-discrimination laws and prohibiting exclusion, adverse treatment, coercion or other discrimination against individuals or entities on the basis of their religious beliefs or moral convictions and does not discriminate on the basis of race, color, national origin, age, disability, or sex. Network Health does not exclude people or treat them differently because of race, color, national origin, age, disability, or sex. You may have the right under federal law to decline to undergo certain health care‐related treatments, research, or services that violate your conscience, religious beliefs, or moral convictions.
Network Health:
Provides free aids and services to people with disabilities to communicate effectively with us, such as:
Qualified sign language interpreters
Written information in other formats (large print, audio, accessible electronic formats, other formats)
Provides free language services to people whose primary language is not English, such as:
Qualified interpreters
Information written in other languages
If you need these services, contact Network Health’s discrimination complaints coordinator at 844-625-2208.
If you believe that Network Health has failed to provide these services, has failed to accommodate your conscientious, religious or moral objection or discriminated in another way on the basis of race, color, national origin, age, disability, or sex, you can file a grievance with Network Health’s discrimination complaints coordinator, 1570 Midway Place, Menasha, WI 54952, phone number 844-625-2208, TTY 800-947-3529, Fax 920-720-1907, compliance@networkhealth.com. You can file a grievance in person or by mail, fax, or email. If you need help filing a grievance, Network Health’s discrimination complaints coordinator is available to help you. You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights electronically through the Office for Civil Rights Complaint Portal, available at https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by mail or phone at U.S. Department of Health and Human Services, 200 Independence Avenue SW., Room 509F, HHH Building, Washington, DC 20201, 1-800-368-1019, 800-537-7697 (TDD). Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html.
If you, or someone you’re helping, has questions about Network Health, you have the right to get help and information in your language at no cost. To talk to an interpreter, call 844-625-2208.
Spanish: Si usted, o alguien a quien usted está ayudando, tiene preguntas acerca de Network Health, tiene derecho a obtener ayuda e información en su idioma sin costo alguno. Para hablar con un intérprete, llame al844-625-2208.
Hmong: Yog koj, los yog tej tus neeg uas koj pab ntawd, muaj lus nug txog Network Health, koj muaj cai kom lawv muab cov ntshiab lus qhia uas tau muab sau ua koj hom lus pub dawb rau koj. Yog koj xav nrog ib tug neeg txhais lus tham, hu rau 844-625-2208.
Chinese: 如果您,或是您正在協助的對象,有關於[插入SBM項目的名稱 Network Health 方面的問題,您有 權利免費以您的母語得到幫助和訊息。洽詢一位翻譯員,請撥電話 [在此插入數字844-625-2208.
German: Falls Sie oder jemand, dem Sie helfen, Fragen zum Network Health haben, haben Sie das Recht, kostenlose Hilfe und Informationen in Ihrer Sprache zu erhalten. Um mit einem Dolmetscher zu sprechen, rufen Sie bitte die Nummer 844-625-2208 an.
Arabic: لديك الحق في الحصول على المساعدة والمعلومات باللغة الخاصة بك ،Health Network إذا كان لديك أو لدى شخص كنت مساعدة، أسئلة حول .2208-625- دون أي تكلفة. للتحدث مع مترجم فوري، قم باستدعاء 844
Russian: Если у вас или лица, которому вы помогаете, имеются вопросы по поводу Network Health, то вы имеете право на бесплатное получение помощи и информации на вашем языке. Для разговора с переводчиком позвоните по телефону 844-625-2208.
Korean: 만약 귀하 또는 귀하가 돕고 있는 어떤 사람이 Network Health 에 관해서 질문이 있다면 귀하는 그러한 도움과 정보를 귀하의 언어로 비용 부담없이 얻을 수 있는 권리가 있습니다. 그렇게 통역사와 얘기하기 위해서는844-625-2208.로 전화하십시오.
Vietnamese: Nếu quý vị, hay người mà quý vị đang giúp đỡ, có câu hỏi về Network Health, quý vị sẽ có quyền được giúp và có thêm thông tin bằng ngôn ngữ của mình miễn phí. Để nói chuyện với một thông dịch viên, xin gọi 844-625-2208.
Pennsylvania Dutch: “Wann du hoscht en Froog, odder ebber, wu du helfscht, hot en Froog baut Network Health, hoscht du es Recht fer Hilf un Information in deinre eegne Schprooch griege, un die Hilf koschtet nix. Wann du mitme Interpreter schwetze witt, kannscht du 844-625-2208 uffrufe.
Laotian: ຖ້ າທ່ ານ, ືຫຼ ຄົ ນທ່ ທ່ ານກໍ າລັ ງຊ່ ວຍເືຫຼ ອ, ມໍຄາຖາມກ່ ຽວກັ ບ Network Health, ທ່ ານມ ິສດທ່ ຈະໄດ້ ຮັ ບການຊ່ ວຍເຫຼື ອແລະຂໍ ້ ມູ ນຂ່ າວສານທ່ ເປັ ນພາສາຂອງທ່ ານບໍ່ ມ ຄ່ າໃຊ້ ຈ່ າຍ. ການໂອ້ ລົ ມກັ ບນາຍພາສາ, ໃຫ້ ໂທຫາ 844-625-2208.
French: Si vous, ou quelqu'un que vous êtes en train d’aider, a des questions à propos de Network Health, vous avez le droit d'obtenir de l'aide et l'information dans votre langue à aucun coût. Pour parler à un interprète, appelez 844-625-2208.
Polish: Jeśli Ty lub osoba, której pomagasz ,macie pytania odnośnie Network Health, masz prawo do uzyskania bezpłatnej informacji i pomocy we własnym języku .Aby porozmawiać z tłumaczem, zadzwoń pod numer 844-625-2208.
Hindi: यिद आप, या िकसी को आप की मदद कर रहे ह, के बारे म सवाल है Network Health, आप कोई भी कीमत पर अपनी भाषा म मदद और जानकारी प्रात करने का अिधकार है। एक दुभािषया के िलए बात करने के िलए, 844-625-2208 कहते ह।.
Albanian: Nëse ju, ose dikush që po ndihmoni, ka pyetje për Network Health, keni të drejtë të merrni ndihmë dhe informacion falas në gjuhën tuaj. Për të folur me një përkthyes, telefononi numrin 844-625-2208.
Tagalog: Kung ikaw, o ang iyong tinutulangan, ay may mga katanungan tungkol sa Network Health, may karapatan ka na makakuha ng tulong at impormasyon sa iyong wika ng walang gastos. Upang makausap ang isang tagasalin,tumawag sa 844-625-2208.